The MGH Today. Photographed by Mike Haimes. Courtesy the Montreal General Hospital Foundation
Introduction
Since the mid-nineties, the MGH has entered an era of increasingly specialized, high-tech, high-touch care, indicative of its role in the McGill university hospital network.
By the turn of the new millennium, hospitals had become more technologically-dependent than ever before. Like other hospitals, the MGH had to plan extensively around the Y2K-based threat of global systems failure. Montreal’s economy had shifted from an industrial centre to a technological and cultural hub with a thriving tourist industry, while the province balanced cutbacks with legislation that brought pharmacare and affordable childcare to the population.
Though the merger presupposed the eventual consolidation of physical sites into a single superhospital, by the time detailed plans were developed for the Glen site it was thought that the MGH would better serve the population as a complementary site, easing pressures on the city’s emergency rooms (Source: Soins, enseignement, recherche au coeur de la cite: Rapport de la Commission d’analyse des projets d’implantation du Centre hospitalier de l”universite de Montreal et du Centre universitaire de sante McGill)
Designed by Linda Jackson
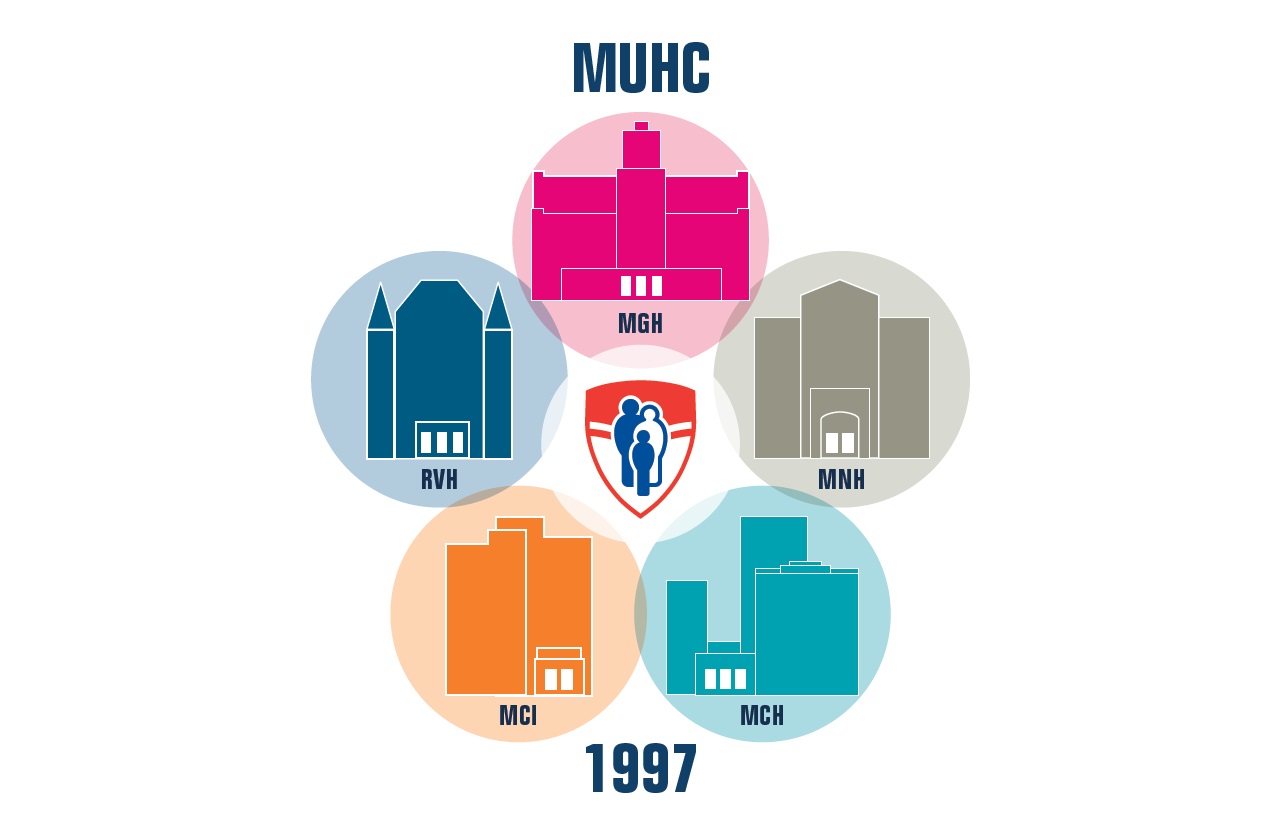
The healthcare sector saw the creation of nineteen integrated networks across the province and the designation of four academic health-science centres. The McGill University Health Centre was formed in 1997 through the merger of five institutions, of which the MGH was the oldest. These academic centres were to play a clearly defined role in the healthcare system, providing ultra-specialized care, groundbreaking research, and education for future healthcare professionals.
Nora Livingston, William Osler, Thomas Roddick and other MGH legends understood that “the patient must come first.” Over the past 200 years, this mantra has set the standards and tone for the evolution of clinical care, teaching and research.
The MGH Today is home to numerous and varied clinical initiatives whose common threads are multidisciplinary teamwork, patient empowerment and innovation. These programs demonstrate the ongoing commitment to and from our community and provide a glimpse of the future.
A Leader in Trauma Care in Quebec and Beyond
The MGH has a well-earned reputation for the quality of its trauma care. When a provincial task-force concluded in 1992 that mortality rates associated with trauma were over fifty percent, the MGH had already adopted a trauma protocol based on the principle that a rapid response could save lives. In 1993, with leadership from the MGH’s David Mulder, these principles were formalized into a province-wide trauma system. The mortality rate of trauma victims who benefited from this service fell from 51.8% to 2.5% between 1992 and 2007.
The Traumatic Brain Injury Program team, 2021. L-R, back row: Alena Seresova, Maude Laguë-Beauvais, Marie-Claude Champoux, Dr. Simon Tinawi, Paulo Fumaneri, Dr. Mohammad Maleki, Diane Bastasi, Christine Gonzalez, Howell Lin, Dr. Judith Marcoux, Gail Brathwaite, Dr. Jehane Dagher. L-R, middle row: Marie-Josée Bernier, Michel Abouassaly, Rosa Rosarini. L-R, front row: Deidra Santos, Tanvir Dhoot. Image courtesy of the Medical Multimedia Department of the MUHC. Photographed by Michael Cichon.
As part of these changes, the MGH was named one of three regional Level 1 Trauma Centres in 1997. This transition was aided by the Desmarais family – longstanding supporters of the hospital. Today, the Montreal General Hospital David S. Mulder Trauma Centre treats an average of 1,600 serious trauma cases a year, with one of the largest multi-disciplinary trauma care teams in North America. In addition, given the complexity of issues facing survivors of trauma, neuropsychologist Mitra Feyz established the Traumatic Brain Injury Program. It consists of a team of rehabilitations professionals who work with patients and families to improve functional outcomes and quality of life, in collaboration with community partners from Montreal, Montérégie and Northern Quebec.
Since 1997, the Mulder Trauma Centre has expanded its reach into local and international communities. Given the large percentage of traumas that are preventable, the trauma team plays an important role in educating the public and has advocated for a safer environment through talks and workshops on subjects such as fall prevention, road safety, gun control and safe sporting practices. On a global scale, the Centre for Global Surgery, co-directed by Tarek Razek and Dan Deckelbaum, has been sharing their knowledge about trauma systems in Africa, Latin America, and the Middle East.
Fertile Testing Ground:
Reproductive Immunology
Geneviève Genest, working out of the MGH’s Division of Allergy and Immunology, established Canada’s first reproductive immunology clinic to test the hypothesis that undetected imbalances in the uterine system play a key role in conception and sustaining pregnancy. She treated a number of patients suffering from unexplained recurrent pregnancy loss with intravenous immunoglobulin (IVIg). IVIg is a concentrated plasma protein made from antibodies drawn from thousands of blood donors that is commonly used to treat a number of autoimmune disorders. The results were extraordinary. In a trial of fifteen women, thirteen were able to have a child after receiving IVIg therapy. Genest is now looking for a non-invasive diagnostic marker to better identify patients for whom this therapy would likely work and she is analyzing immune cells before and after IVIg therapy to link this to success or failure.
Mental Health at the MGH
Prior to 1946, the treatment of psychiatric disorders at the MGH fell under the umbrella of the Department of Neurology, though most individuals were institutionalized separately in facilities such as the Saint-Jean de Dieu Hospital, and the Verdun Protestant Hospital for the Insane (now the Douglas Institute for Mental Health).
Modern psychiatric treatment was established at the MGH in the direct aftermath of WWII, which had highlighted the prevalence of psychiatric issues among the general population. In 1946, Albert E. Moll, the MGH’s first Psychiatrist-in-Chief, began outpatient consultations at the Western and Central divisions of the MGH. Under Moll, the department was at the forefront of community-based mental health care, which became the primary axis of care for psychiatric patients after the deinstitutionalization movement of the 1960s.

The Day and Night Centres (opened in 1950 and 1954, respectively) were pioneering programs established to meet the increased demand for psychiatric outpatient services.
Group Therapy, Night Clinic, Department of Psychiatry of the MGH. Art and Heritage Centre of the MUHC, Mann Fonds, 2017-0001.04.59
Today, the Mental Health Mission is a wide-ranging, multifaceted service that reflects current-day understandings of the mental health spectrum and its complexities. Building on a legacy of teamwork, the Mission combines the Departments of Psychiatry and Psychology, working with doctors, nurses, occupational therapists, social workers, and other allied health professionals. It provides in- and out-patient services, specialized emergency and acute care, and liaison consultation to a wide variety of hospital services and departments.
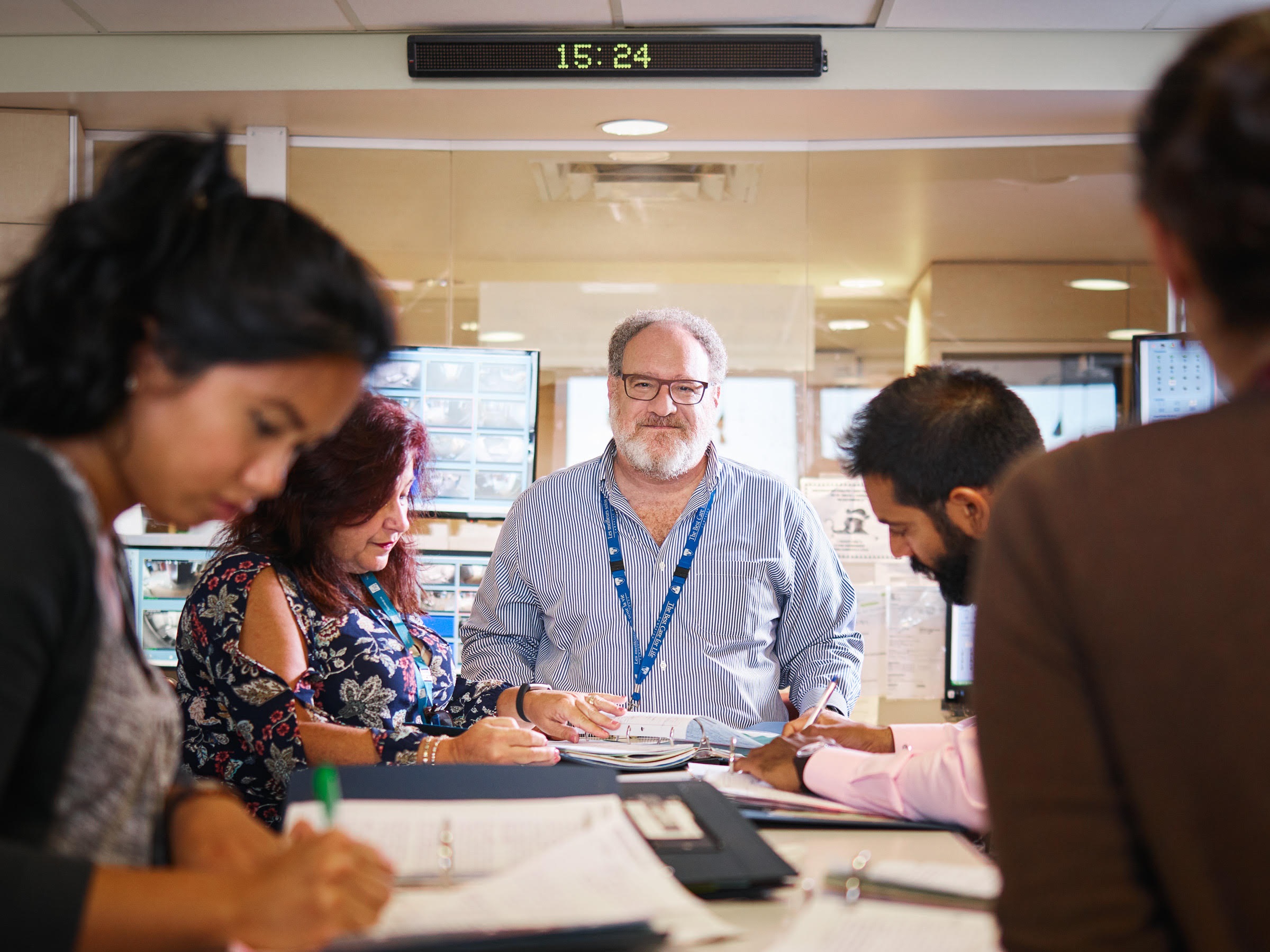
Dr. Warren Steiner, psychiatrist with the Mental Health Mission, at the MGH. Image courtesy of the Montreal General Hospital Foundation.
The Mental Health Mission uses patient empowerment, cutting edge therapies, prevention and early intervention, as well as programs tailored to meet the diverse needs of the community, such as:
- the McGill University Sexual Identity Centre (MUSIC), an award-winning psychotherapeutic service for LGBTQI+ patients and their families;
- a neuromodulation unit, which offers cutting-edge rTMS (repetitive transcranial magnetic stimulation) therapy for medication-resistant illnesses;
- Cognitive Behavioural Therapy and Psychopharmacology and Therapeutics units;
- The Recovery Transition Program, which harnesses the experiential knowledge of recovered/recovering patients towards a self-sustaining, volunteer-led program geared towards patient empowerment and integration back into the community;
- Specialized programs for substance abuse, anxiety disorders, first episode psychosis, mood disorders, and personality disorders.
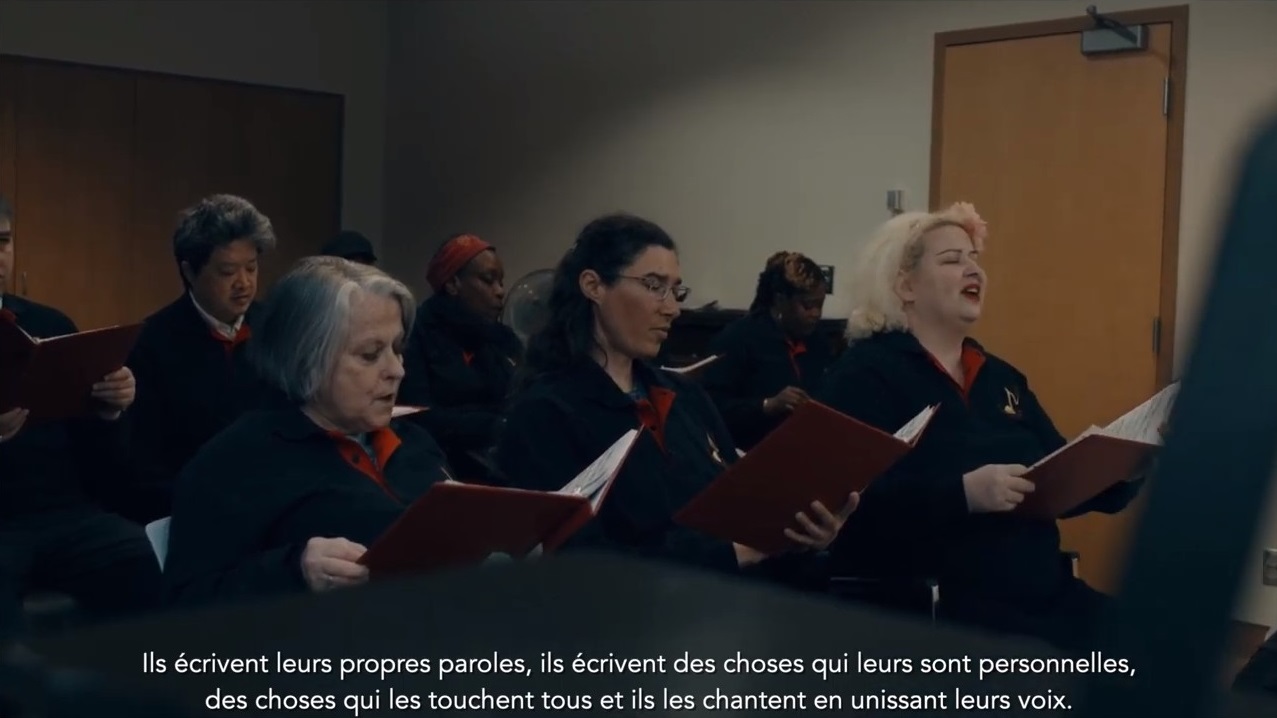
Community Support
The Mental Health Mission is also a remarkable example of the impact of community support through fundraising, volunteering and philanthropy, supported by long term MGH donors and volunteers alike. The Angus family, which has supported the MGH since the 1960s, funds a variety of programs and therapies, including the Jacqueline Angus Psychiatric Emergency Department and Brief Intervention Unit, music therapy, psychopharmacology, recovery transition, and research into severe psychiatric diseases.
Peri-operative Program (POP):
Empowering Patients through Prehabilitation
Founded by Dr. Franco Carli, an anaesthesiologist, the Peri-Operative Program (POP) is one of the first prehabilitation programs in North America. The POP funnels a network of resources and therapies – such as kinesiology, nutrition, and psychoeducation – towards supporting patients during pre-surgical wait times. These resources empower patients to be proactive about their pre-surgical fitness, while also providing the structure, supervision, care and attention required for success.
The program’s success rate demonstrates the value of investing in patients’ desires to improve and empower themselves. Studies have shown that 80% of POP patients achieve their pre-surgical baselines with prehabilitation, compared to 50% with rehabilitation, and 35% with no intervention. In 2020, Dr. Carli was elected chairman of the American Prehabilitation Society and received international recognition for his pioneering work.
Thoracic Oncology :
Precision care for the deadliest cancers
Techniques utilized by the Division make use of an extensive biobank of living tissues. These enable the team to pinpoint the most effective drug therapies. The Division is also home to the first phase 3 trial in the world that uses immunotherapy prior to cancer surgery, which has doubled the survival rate of many Stage Four lung cancer patients.
Described by Lorenzo Ferri, Chief of the Division of Thoracic Surgery, as a “one stop shop” for complex cancer care, the Division boasts an integrated surgical and research platform that enables it to push the limits of cancer research in entirely new directions. Innovative treatments are geared towards improving patient care. Usng recent technological advancements, they are tailored to individual patients’ biological makeups to move cancer treatment beyond a “trial and error” model, which can be devastating.
Chronic care :
The Inflammatory Bowel Disease (IBD) program
The program affords patients the benefit of continuous, individualized care over a long period of time – a crucial element in a program geared to managing a chronic, incurable illness. It also provides access to clinical trials in the emerging field of IBD treatment, and a direct line to urgent care.
COVID-19 at the MGH

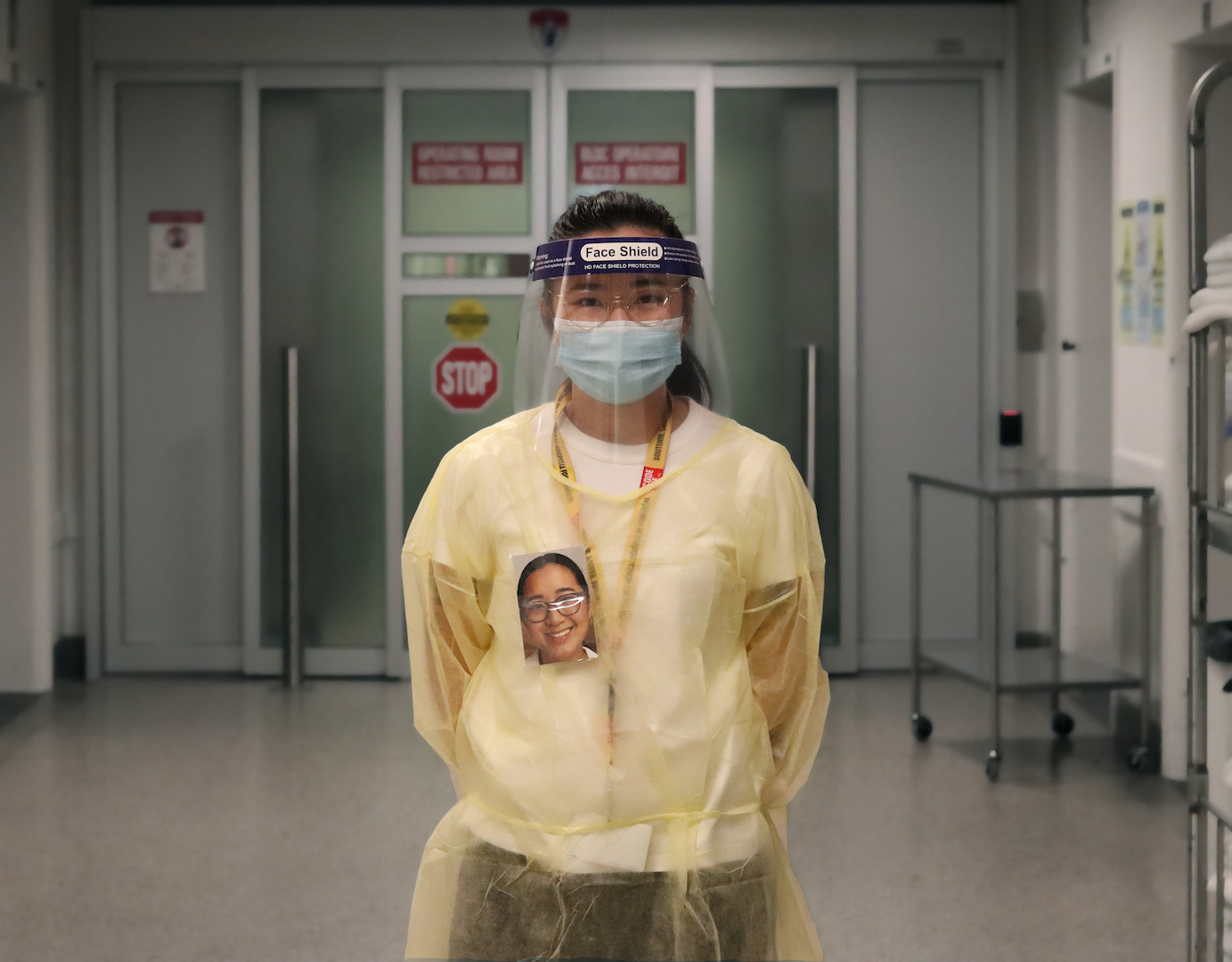
PPE Portraits are a hybrid art and medical intervention designed to improve patient care and team dynamics by humanizing the alienating appearance of PPE with the use of warm and smiling headshots.
Geneviève Lambert, kinesiologist, MGH Peri-Operative Program, wearing a PPE (Personal Protective Equipment) portrait, 2021. Photo by Laura Rendon and Geneviève Lambert.
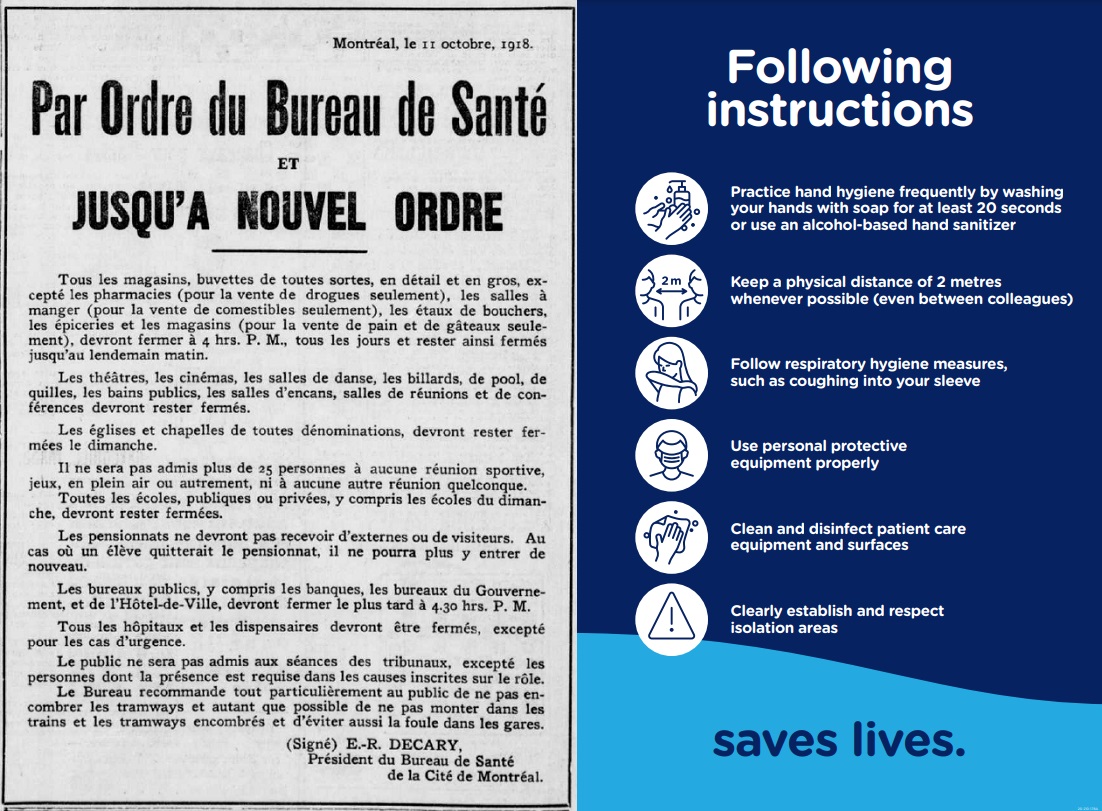
When the 1918 Influenza pandemic arrived in Montreal, the MGH was already nearing its one hundredth birthday. At the time, the hospital responded to the city’s infection surges, despite severe staff shortages caused by the World War One and exacerbated by the pandemic. The MGH also consulted on the opening of a temporary hospital near the port to treat soldiers returning home.
One hundred years later, the MGH is again living through historic times, along with the rest of the world. While the 1918 Influenza initially spread between continents with flows of military traffic, today’s COVID-19 has largely spread globally through air travel in an increasingly connected, cosmopolitan world. Both in 1918 and today, the city resorted to masks, distancing, and shutdowns of public gathering spaces to slow transmission of the disease. While it took decades for the world to develop an influenza vaccine, next-generation vaccine platforms have made it possible to develop effective vaccines for COVID-19 in under a year, using nucleic acid-based (RNA) methods.
As was the case in 1918, health care workers have been tireless in their effort to treat and limit the spread of COVID-19, providing humane care and setting an example for the rest of society. Their service to the community during this crisis marks another heroic chapter in the hospital’s history.
Code Life Ventilator Challenge
Recently, the MGH Foundation teamed up with the MUHC Research Institute to launch the Code Life Ventilator Challenge. Against the backdrop of a looming ventilator shortage due to rising cases of COVID-19, they launched an international contest that called on designers to develop prototypes for ventilators that could be easily and cheaply produced. The response was overwhelming: over one thousand applicant teams from all over the world entered the contest. The Ventilator Challenge also acts as a bridge between designers and manufacturers, and has raised extra funds to work with companies to help with production and maintenance.
Out of three finalists, Montreal robotics company Haply won the design contest for their easy-to-source design utilizing 3D printers.
Longstanding Family Support
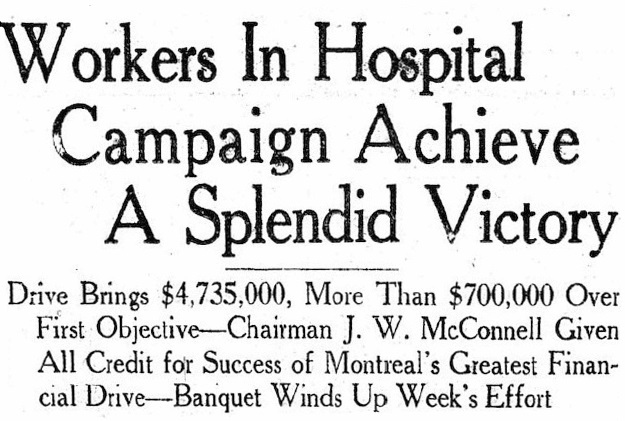
The MGH has survived and thrived thanks to two centuries of community support – from confiscated fish donated by the game inspector, to major fundraising campaigns chaired by members of Montreal’s most distinguished families.
Among these, two families in particular have, after many decades, continued to support the hospital. J.W. McConnell was a regular and generous contributor to the Montreal General Hospital, and, since its founding, the Foundation that carries his name has continued that legacy. The Foundation’s contributions have helped advance research in numerous areas, including pain treatment, cancer, mental health and ileitis and colitis. Funding has also gone to support practical medical training and to ensure the sustainability of critical academic positions.
John W. McConnell at his desk, Dominion Express Building, Montreal, QC, ca 1935. McCord Museum, M2003.8.6.5001
The Molson family has supported the MGH for seven generations, beginning with John Molson, Sr. mounting the very first argument in support of a public hospital at the legislative assembly of Lower Canada in 1818. This led to the construction of the first Montreal General Hospital, around which Molson Sr. erected an ornate wrought iron fence. The new building was constructed in 1953 using many of the same materials as the Molson Brewery, including the exterior brick. The Molson family also helped establish the Montreal General Hospital Foundation in 1973.